As a result of rising healthcare costs, there have been widespread efforts to reform healthcare delivery worldwide. To succeed in this, many hospitals, health systems, and independent clinics are turning to clinical integration.
Clinical Integration – What is it and Why Do We Need it?
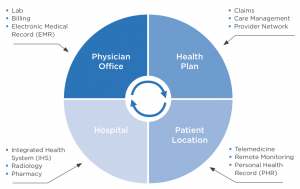
Over the last few decades, the mode of healthcare delivery has shifted from a traditional inpatient model to increasing use of outpatient services. This trend has been facilitated by technological advances making it easier for inpatient providers to move their patients to outpatient facilities. In turn, this has led to separation of hospital services, with patients who require coordinated care often seeing multiple providers. To support this practice, each patient’s medical information must be documented using longitudinal records that are accessible to all authorized providers at the point-of-care.
However, despite the technological advances and the promise outpatient care holds for improving outcomes, clinical information is often not effectively shared between different providers, forcing them to rely on incomplete patient or family collateral. As a result, this negatively affects the patient outcomes (and thereby costs). To overcome these issues and enable healthcare reform, clinical integration, both within and across organizations (“vertical” and “horizontal” integration, respectively), needs to be top priority.
 The American Hospital Association defines “clinical integration” as a way to improve coordination of patient care across different conditions, providers, settings, and time. By doing so, we can achieve safe, timely, cost-effective, patient-focused, high-quality care. However, there must first be changes in provider culture, payment methods, and incentives, as well as modernization of federal laws.
The American Hospital Association defines “clinical integration” as a way to improve coordination of patient care across different conditions, providers, settings, and time. By doing so, we can achieve safe, timely, cost-effective, patient-focused, high-quality care. However, there must first be changes in provider culture, payment methods, and incentives, as well as modernization of federal laws.
Key Components of Clinical Integration
To achieve clinical integration, we need the following:
- An integrated platform enabling access to patient clinical data for all providers
- Collection of data on cost, program utilization and participation, and clinical outcomes
- Retrospective and predictive analytics
- Ongoing collaboration and communication between in- and outpatient providers, including both primary care physicians and specialists. This should include information on the setting of care delivery, the assessments and treatments given, and the treatment plan going forward.
- Coordination of management of complex cases and between providers and disease-management programs
- Case managers assigned to each complex or chronic patient; these should be responsible for discharge planning from the time of admission.
Benefits and Potential Outcomes of Clinical Integration
Clinical integration has multiple benefits for healthcare, including:
- Improved quality and continuity of care
- Improved quality- and financial monitoring
- Better operational efficiency
- Improved patient experiences and clinical outcomes
- Lower care costs and better cost-effectiveness
- It allows for more comprehensive medical information to be shared
- It allows focus to be placed on preventive medicine rather than treating acute events
- Strengthening of relationships among different providers
- It can make providers more attractive network participants to payers
- Sustained independence for physicians in smaller or private clinics
- It positions providers to take on higher levels of accountability
Below, I explore some of these benefits in more detail.
Improved Operational Efficiency
Successful implementation of a clinical integration system improves operational efficiency by highlighting key performance issues related to poor quality outcomes and inefficient resource utilization and care. Consequently, clinical integration ensures better coordination of healthcare services and thereby more consistent and higher-quality care, as well as improved cost management.
An integrated system that incorporates clinical decision support and alerts can moreover provide continuous feedback to the providers. The documented data can be compared against quality indicators and be used to determine if the established procedures for quality improvement were utilized.
More Comprehensive Medical Information
Clinical integration allows bundling of data into a shared platform, providing a longitudinal care record. This results in more up-to-date and comprehensive clinical information and medical histories. In turn, this allows the different providers to more efficiently determine the treatment strategy going forward based on past results. Additionally, advanced functionalities such as clinical decision support, where the data can be compared to evidence-based practices, allow providers to examine established clinical pathways and receive best-practice alerts. Integrated systems can also provide information about clinical guidelines and pathways specific to a condition, as well as clinical reminders about important quality measures/recommendations at the point-of-care.
Hence, clinical integration facilitates tracking of healthcare measures and involvement of the care team in providing information about patient progress. In turn, having more comprehensive medical information results in more appropriate management of the patients. This is especially true for patients with chronic conditions, who often see a range of healthcare providers, both in the in- and outpatient settings.
Quality Monitoring
Through clinical integration, data for quality monitoring can be more easily accumulated. These data can then be used by patients to help them choose the highest quality, most cost-effective, and/or most readily available care. At the same time, an integrated system can also help provide feedback to the providers to ensure continuous improvements to the quality of care. Thus, hospitals and clinicians can use the same data to measure their own performance and improve their financial health. Consequently, the overall care and health of the patients will improve.
Improvements in Patient Care
As alluded to above, one, if not the, greatest benefit of clinical integration is the improved patient care that ensues. When patients are tracked as they move through different providers, the risks of medication errors, duplicate testing, unnecessary readmissions, and conflicting treatment strategies are minimized.
Clinical integration also promotes the sharing of best practices and care standards, along with system-wide data collection. This can then guide future treatment decisions and identify emerging trends. In addition, clinical integration facilitates preventive medicine and proactive treatment by allowing each provider to become aware of any issues before the patient comes in for an appointment. Thereby, they can anticipate and prevent any problems before they arise or worsen.
Further, “clinical alert” reminders regarding a patient’s status can suggest evidence-based treatment courses to providers. Together with their own judgment and expertise, these suggestions can subsequently be incorporated when determining the most appropriate clinical care pathway. Later, the way care was actually provided vs. the evidence-based suggestions from the alerts and decision support tools can be compared when retrospectively examining the patient outcomes. This helps determine if additional procedures or a different treatment protocol should have been used.
New or Improved Reimbursement Models
With the passage of the Affordable Care Act in 2010, the US healthcare system is slowly moving toward a model where reimbursement is based on improved outcomes and cost-efficiency rather than the number of patients seen. Disparate medical record systems cannot stand alone, as this makes it difficult to meet the required reporting needs. Hence, clinical integration is instrumental to facilitate significant changes to the current reimbursement model. Especially, it is needed to provide continuous, as well as retrospective, feedback. Accordingly, an integrated system must contain the functionalities for these changes. Moreover, for any given patient or treatment, an integrated system is needed to ensure that the quality thresholds are met and that the cost falls below the bundled payment amount.
Healthcare Reform
As mentioned, clinical integration is critical for healthcare or payment reform, including to address rising healthcare costs and suboptimal patient outcomes. Moving towards clinical integration before implementing large-scale reforms enables organizations to work together to address these issues. Subsequently, this helps minimize the initial costs and workflow disruptions associated with abrupt changes to a system. The clinical integration process typically involves approaching healthcare from a more holistic approach to better coordinate the care of each patient. In particular, to prepare a hospital or clinic for payment reform, there needs to be a standardized electronic medical record (EMR) system to allow seamless sharing of a patient’s clinical, administrative, and financial data.
Changing a payment system is far from simple. For example, there are frequently questions on how to best measure quality of care, and what incentives to provide to improve the quality. A lack of data standardization, missing data, and other issues surrounding the implementation of administrative and process requirements often limit national programs working towards healthcare reform. Clinical integration can help overcome these issues in several ways, including:
(1) By creating standardized datasets from where physicians, patients, or organizations can obtain quality measures.
(2) By providing a platform allowing easier implementation of value-based reimbursement programs.
(3) By creating a system that makes healthcare services more affordable, allowing the reimbursement rates to remain the same or decrease, without negatively impacting the providers’ income.
Importance of a Standardized EMR System for Healthcare Reform
 Having one major EMR platform across a care network allows seamless and secure information transfer between different information systems. Further, a care coordination platform that pulls data from disparate EMRs and transforms the data into the preferred format to create a single patient EMR can supplement such a system. As a result, all network providers know what information will be shared and where to share it.
Having one major EMR platform across a care network allows seamless and secure information transfer between different information systems. Further, a care coordination platform that pulls data from disparate EMRs and transforms the data into the preferred format to create a single patient EMR can supplement such a system. As a result, all network providers know what information will be shared and where to share it.
Before integration, however, it is important to address potential human-computer interface problems. Poor or inconsistent EMR interfaces can exacerbate the workflow challenges related to integration. For example, too many tabs or too much information on each tab can overwhelm the users, making it difficult to quickly determine what clinical information is relevant at each treatment step. Therefore, a robust and clean interface design, allowing each provider to easily filter the data, is of utmost importance.
Nevertheless, it is also important to be able to access each patient’s entire care record to understand their past and current diagnoses and treatment plans. Thus, complete and longitudinal information must be located within the EMR to allow a comprehensive understanding of the patient’s condition and to determine the best treatment course.
Analytics for Clinical Integration
Another important component of clinical integration for healthcare reform is analytics. This provides a consolidated view of the research, clinical, financial, and administrative factors needed to measure accountability, performance, and quality. To this end, organizations must consider the views of the hospital, individual providers, patients, and the population as a whole. Broadly, there are two types of analytics: retrospective and predictive. The former analyzes past patient data for disease or population health management and is useful for assessing the clinical or operational performance of a healthcare or payment system. On the other hand, the latter uses current and past data to make predictions regarding a patient’s future health status and determine the most appropriate care pathway. Together, the two can highlight the level of care provided to a patient and help determine the appropriate bundled payment for their diagnosis and/or treatment.
Health Information Exchange
Considering the cost of, and disruption from, merging or replacing disparate EMR systems into one single infrastructure, an alternative approach has emerged in recent years. Namely, health information exchange (HIE). HIE allows physicians and other healthcare providers to securely access and share a patient’s medical information electronically, within or across organizations, even when the information comes from multiple databases. As an alternative to EMR consolidation, HIE provides several benefits for achieving clinical integration, including:
- Improved speed, quality, and safety of patient care by reducing medication and medical errors, and unnecessary testing
- Reduced health-related costs
- More efficient point-of-care decision support and analytical applications
- Better consumer education and patient involvement in their own healthcare
- Improved efficiency by eliminating unnecessary paperwork for both providers and patients
- Improved public health reporting and monitoring
- More efficient care by enabling automatic appointment reminders and/or follow-up instructions to the patients, and prescriptions sent directly to pharmacies
- Creation of a potential feedback loop between health-related research and real-life practice
- More efficient deployment of emerging technology and healthcare services
- Provision of technical infrastructure that both national and regional initiatives can leverage
Lastly, HIE provides a basic level of interoperability among EMRs maintained by individual physicians and organizations. Once this process and the shared data have been standardized, the data can eventually be transferred into a single EMR system. Consequently, this further improves patient care and facilitates clinical integration.
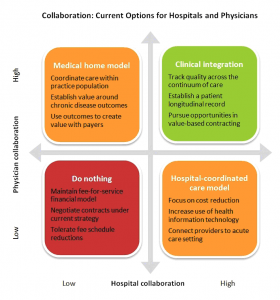
Need for Physician and Administrative Leadership
For healthcare reform to take place, there is moreover a need for physician leadership and transparent physician-hospital communication. To successfully implement a project of this size, health systems looking to pursue clinical integration must therefore empower physician leaders to influence the future direction of the network. After creation of a clinical integration system, physician leaders should participate on the relevant boards and committees working to achieve the program objectives. To ensure physician engagement and encourage ongoing dialogue, there needs to be clear communication strategies, goals, and objectives.
In addition to face-to-face meetings, virtual working groups or advisory boards can facilitate ongoing collaboration and communication with physician leaders and other key stakeholders. To this end, Impetus Digital can help at each step of the way. Using our innovative Impetus InSite Platform, the advisors or working group members are engaged through a series of online touchpoints. These can either be in the form of real-time web meetings or online asynchronous assignments delivered as survey questions via InSite Surveyor, discussion questions via InSite Exchange, debates, case studies, or annotation exercises. The virtual nature of the boards and working groups can help greatly increase the engagement rates of the advisors. Moreover, the assignments can give the advisors time to pause, reflect, process, and review their colleagues’ comments on their own time. In turn, this allows for more thoughtful and granular insights shared through the online forums.
References
American Hospital Association. (2019). Clinical Integration. Retrieved from https://www.aha.org/websites/2012-09-12-clinical-integration
Continuum Health. (2014). Driving Value Through Clinical Integration. Retrieved from https://www.continuumhealth.net/driving-value-clinical-integration/
Goldwater, J., Yuhasz, L. (2011). Considerations for Clinical Integration. Truven Health Analytics. Retrieved from http://truvenhealth.com/portals/0/assets/HOSP_11363_0712_ClinicalIntegration_WP_Web.pdf
HealthIT.com. (2017). HIE Benefits. Retrieved from https://www.healthit.gov/topic/health-it-basics/hie-benefits
HealthIT.com. (2018). What is HIE? Retrieved from https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/what-hie
Marino, D.J. (2012). The 4 Pillars of Clinical Integration: A Flexible Model for Hospital-Physician Collaboration. Becker’s Hospital Review. Retrieved from https://www.beckershospitalreview.com/hospital-physician-relationships/the-4-pillars-of-clinical-integration-a-flexible-model-for-hospital-physician-collaboration.html
Strilesky, M. (2012). The 7 Components of a Clinical Integration Network. Becker’s Hospital Review. Retrieved from https://www.beckershospitalreview.com/hospital-physician-relationships/the-7-components-of-a-clinical-integration-network.html